Hello again. Today’s post is all about how I arrived at my GATA2 deficiency diagnosis. The path, the tests, and everything in between. In hindsight, it was a relatively straightforward sequence of escalating tests, but it still involved many appointments, many doctors, and more blood draws than I think any one person should reasonably be subjected to.
Disclaimer: As always, I want to emphasize that I’m a patient, not a doctor or medical professional. This is simply the path that led to my diagnosis; yours may look different. If you have concerns about your health or questions about your condition, please speak with your medical team
March-September 2024
The awareness of my condition and the early diagnosis that followed is owed, in large part, to a man I’ve never met: Dr. Peter Attia. You may have heard of him or at least had one of his podcast clips forced upon you by the algorithm, if we happen to live in the same corner of the internet. In March of 2024, I picked up his book Outlive and read through it for the first time.
Originally published in 2022, it’s essentially an operating manual for anyone interested in longevity. In it, he argues that while increasing lifespan is a worthy goal, improving the quality of those years matters just as much. For this, he uses the term “healthspan,” which he loosely defines as: ‘the period of life spent in good health, free from the chronic diseases and disabilities of aging.’

I could easily spend entire posts breaking down his book and his ideas, but I think it’s best if you hear it straight from the source. If you’re curious, I highly recommend picking up a copy of the book. You won’t regret it. I’ll include a link to the book below, along with a link to his website if you’d like to learn more about him and his work.
Amendment: While the impact this book has had on my life is difficult to fully measure, I am deeply disappointed in the author as a person due to his recently disclosed involvement with the late Jeffrey Epstein. This mention is not an endorsement of the individual, even if I still believe the book contains information that many people could benefit from. His actions are inexcusable and indefensible. – Ethan (February 2nd, 2026)
Shortly after finishing Outlive, I scheduled my annual physical. I wasn’t particularly worried because just a few months earlier, in October 2023, I’d run my first marathon alongside my brother. As humbling as it was, I felt more confident in my body than ever before. I mean, if I could run a marathon, surely nothing concerning could be happening inside my body… right?

Toward the end of my physical, I asked to get bloodwork done. As a healthy twenty-something, I’d never really had a reason to do it before, but it’s one of the key yearly preventive testing measures that Peter Attia recommends in Outlive. I fully expected the results to reflect how I felt: strong, healthy, and on the right track. Below is the first set of results I received in April 2024.
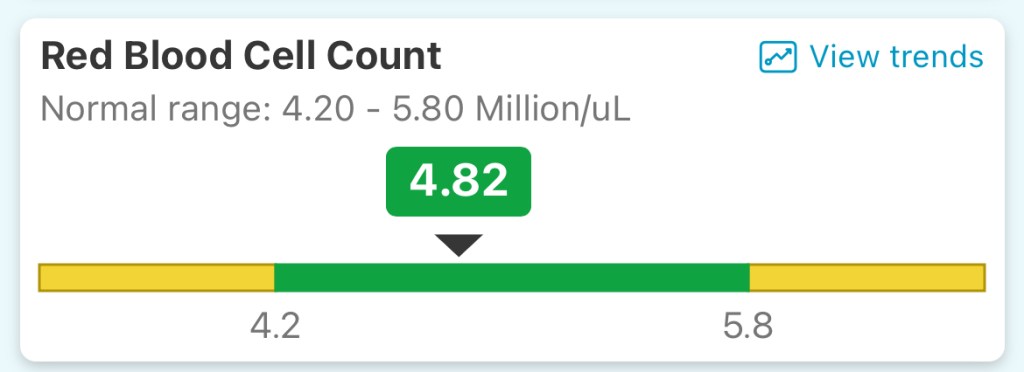
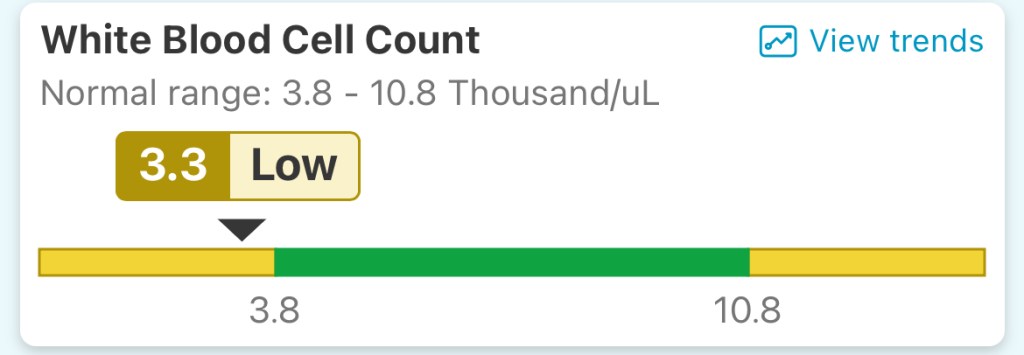
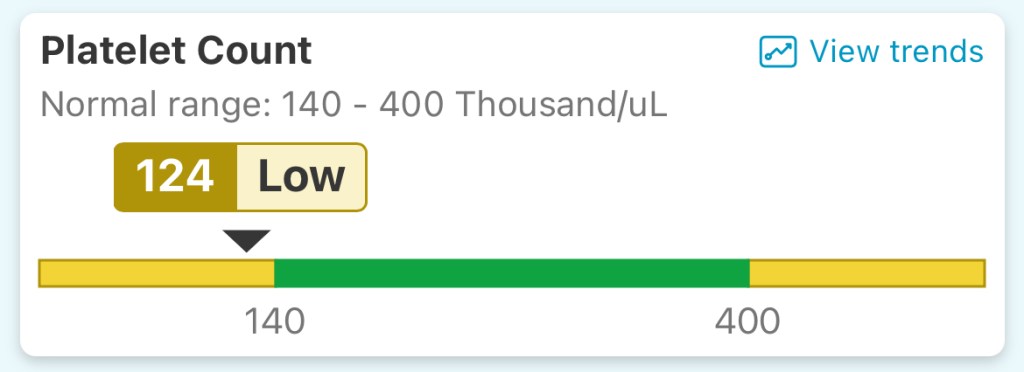
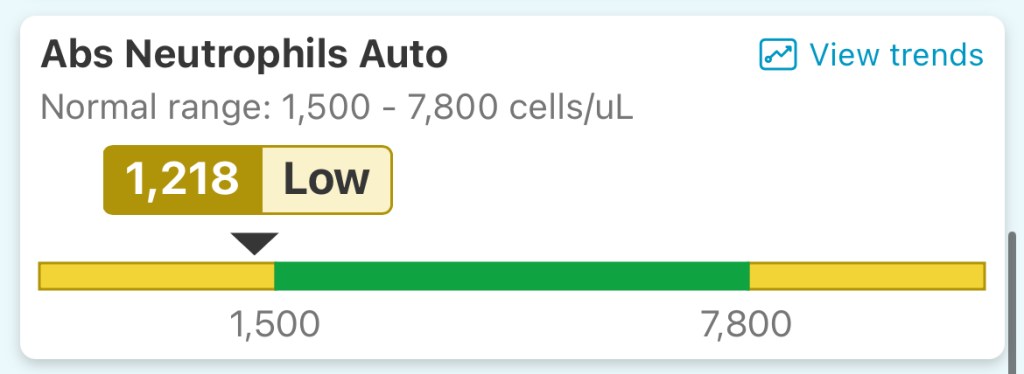
As you can see, there is nothing all that alarming, just slightly low counts in my white blood cells, platelets, and neutrophils. Many doctors may have shrugged this off, but these results are what set everything in motion for me. My primary care doctor recommended following up in about three months, just to be safe. She reassured me that there was no major cause for concern at that time. I followed instructions, and got tested again roughly four months later.
I’ll be sharing a separate post next week about my current health, including full graphs that show how my cell counts have trended over the past year. But for now, just know the follow-up results echoed the first.
October-November 2024
From there, I was referred to a local hematologist in October 2024 for further testing. At the time, I still wasn’t all that worried. 2024 was shaping up to be the healthiest year of my life. Just a week or so before my first appointment, I ran my fastest half marathon ever and was feeling on top of the world. A month before that? My fastest ever 5k. I was fitter and happier than I’d ever been.


My first appointment was primarily a consultation where we outlined the plan for further testing. I felt an immediate trust in my doctor and was eager to dig deeper into what was happening. Following the appointment, they drew more blood and ran a complete blood count (CBC), a comprehensive metabolic panel, and a series of other tests checking things like vitamin levels and lactate. Below are screenshots of my metabolic panel results from that visit that will hopefully give you a better idea for what a metabolic panel actually consists of.
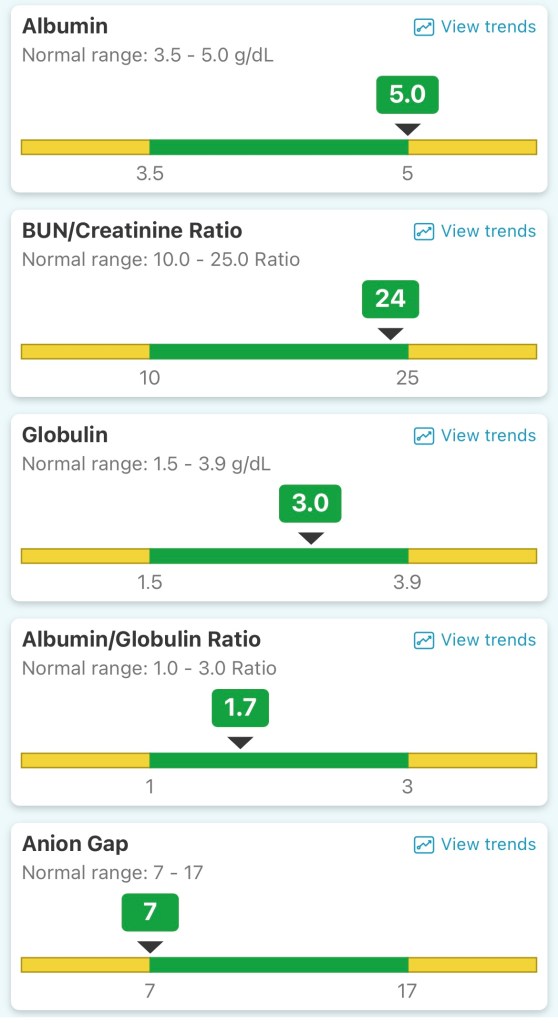

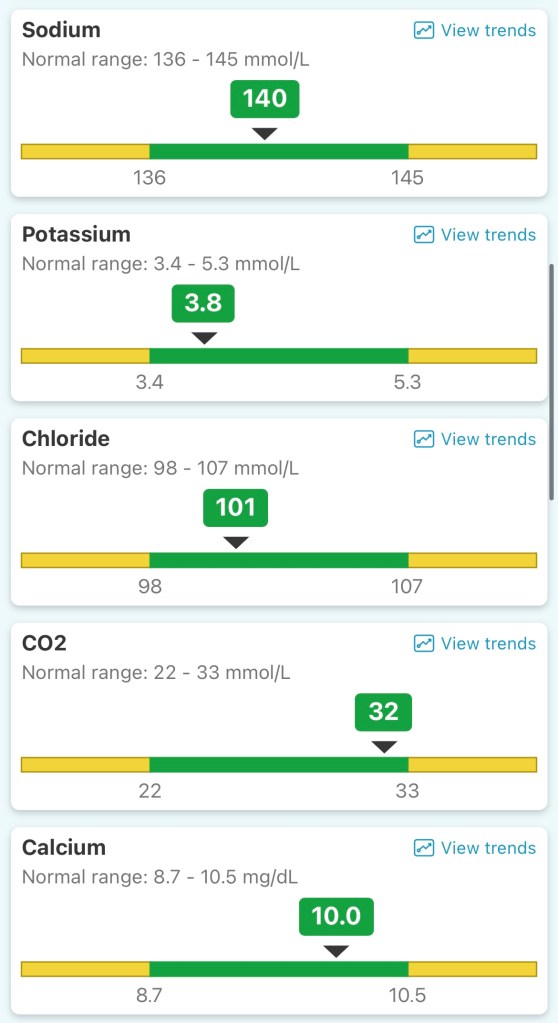
On the whole, my results came back relatively stable, but my counts were still low in a few areas outside of my metabolic panel. We decided to start with my vitamin B12 level. As you will see, I was within a “normal range” for vitamin B12, but a deficiency in this vitamin can actually cause abnormalities in your bloodwork results, so we decided to start there. For the next month or so, I made weekly trips to get vitamin shots.
Not wanting to misrepresent an entire vitamin, I’ll defer to the real experts at the Cleveland Clinic, who state: ‘Vitamin B12 deficiency happens when your body is either not getting enough or not absorbing enough vitamin B12 from the food that you eat that it needs to function properly. Vitamin B12 is an important nutrient that helps your body make red blood cells and DNA, the genetic material in all of your cells. Untreated, vitamin B12 deficiency can cause physical, neurological and psychological problems.’
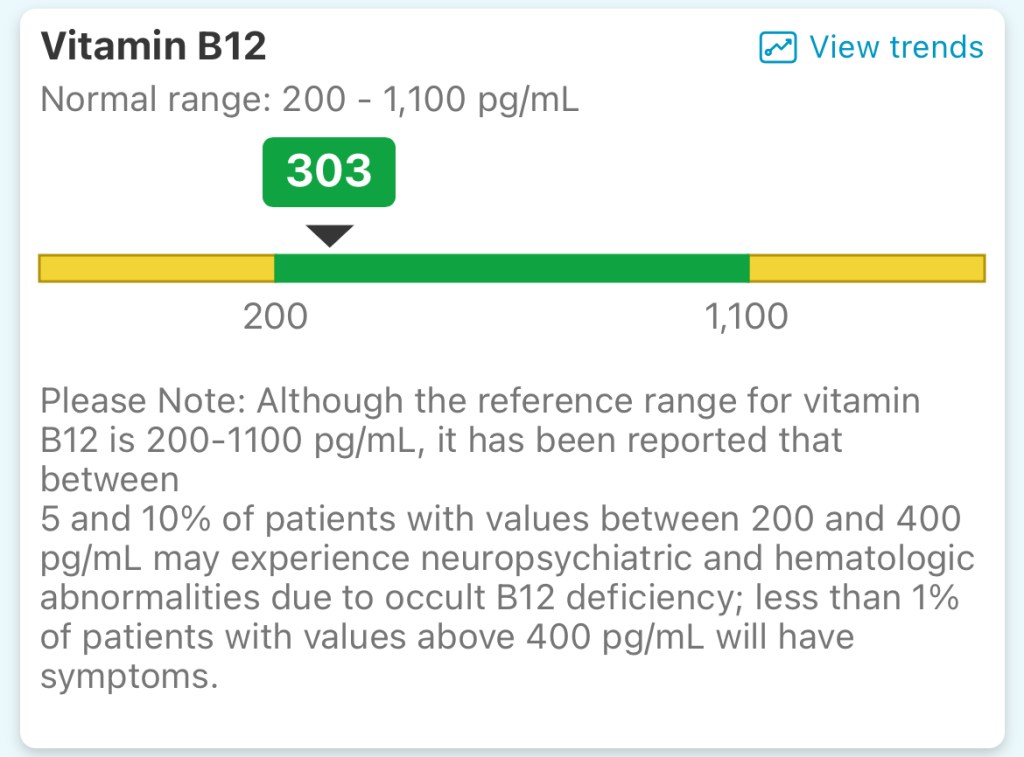
Around that same time, I also had an ultrasound of my spleen. The thinking was that my body might be producing enough cells, but they could be getting trapped there, a phenomenon called ‘splenic sequestration,’ which sounds every bit as enjoyable as it doesn’t. As you might have guessed though, neither of these were the culprits behind my low cell counts. The ultrasound came back normal, and while my vitamin B12 levels improved, my cell counts didn’t budge.
December 2024
Here’s where I started to get more concerned. Not full-blown panic yet, but it was clear that we had moved beyond the ‘easier’ explanations for my low counts. The more testing I went through, the more it dawned on me that something might actually be wrong.
At my next appointment with the hematologist, she explained that we had two more tests that we could run, starting with an antinuclear antibody test (ANA). According to the Mayo Clinic, ‘An ANA test detects antinuclear antibodies in your blood. Normally, your immune system produces antibodies to fight infections, but antinuclear antibodies mistakenly target your body’s own tissues, specifically the nuclei of your cells. A positive ANA test usually means your immune system is attacking your own tissues, signaling an autoimmune reaction.’
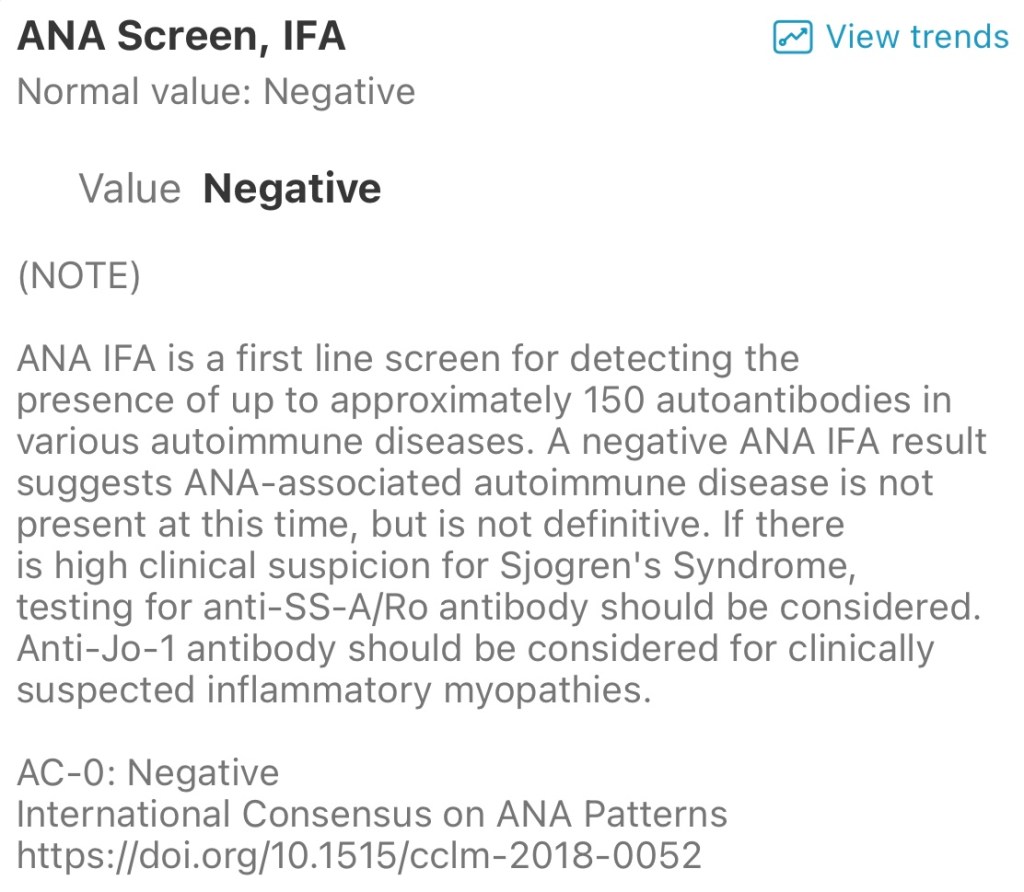
Anyone with an autoimmune disease will tell you they’re no joke. Some can be managed, but most aren’t curable. Your body basically wages war on itself 24/7—not exactly ideal. I didn’t want that ANA test to come back positive, but I also knew we were running out of possible explanations. Before we received the results, my hematologist warned me that if the ANA was negative, the next step would be a bone marrow biopsy. If the immune system wasn’t the culprit, then the explanation was probably buried in my bone marrow.
It was. I had my first bone marrow biopsy on December 18th, 2024. Just a few days before my biopsy, I took a trip to New York City with my mom. We used to go every December, but COVID had put that tradition on pause so this was our first visit back in years. The trip helped take my mind off the looming test and everything it could mean. If there was an issue, what kind? And if everything came back normal, how would we explain the abnormalities in my bloodwork? No good answer either way. It felt like a medical Catch-22.





During my biopsy my hematologist had walked me through why we were doing it and what exactly they’d be looking for. She explained that certain bone marrow issues can be caused by genetic mutations, “some better than others,” as she put it. To be clear, she wasn’t implying there’s such a thing as a good mutation. But given the circumstances, I believe she was doing her best to ease my mind and I’ll always be grateful to her for that.
January 2025
When she called two weeks later on January 2nd, 2025, she said, “This is not one of the better ones.” The biopsy had revealed a mutation in my GATA2 gene, something known as GATA2 deficiency. I responded, “What did you call me?” Just kidding. Sort of. GATA who was doing what, now?
From there, I spiraled. Fully and unapologetically. A completely reasonable reason to crashout, if you ask me. In hindsight, I’m honestly surprised it wasn’t worse. I spent the next month digging for anything I could find about GATA2 deficiency, which, as it turns out, doesn’t take long. A quick Google search will show you just how little clear or consistent information exists about this condition.
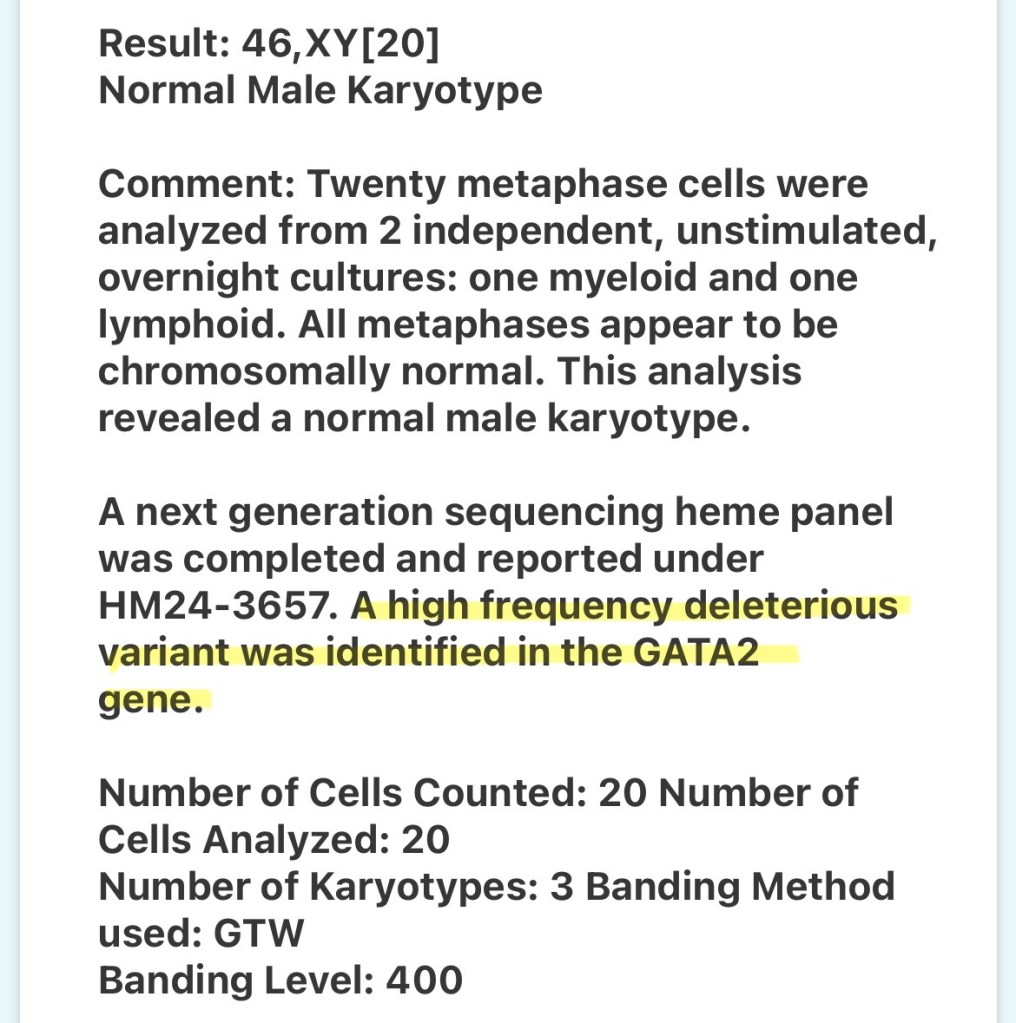
Shortly after my results came back, I was referred to the Hartford Hospital Cancer Center in Hartford, CT, where I met my new local care team. The conversation quickly shifted toward stem cell transplant. While the genetic mutation was the root diagnosis, it was already affecting my bone marrow in ways that raised concern about it potentially progressing into something more serious. At the time, the two possibilities they mentioned were Aplastic Anemia or MDS. Essentially, the mutation was already chipping away at me in ways that concerned my care team enough to want to start the conversation about treatment options.
Unfortunately, Hartford doesn’t have a stem cell transplant program. Fortunately, living in New England means I’m near two of the best transplant centers in the world: Memorial Sloan Kettering in New York City and Dana-Farber in Boston. Since Hartford Healthcare is part of the cancer alliance with MSK, I was referred there and had my first appointment in late January.

Up to this point, I hadn’t found any clear consensus online on whether my condition was curable. Not exactly the most comforting place to be. Those weeks were rough. Sitting with that kind of uncertainty was unlike anything I’d ever experienced. What made it all the more jarring was that I had just finished what I’d consider the healthiest year of my life, only to have life throw me a total haymaker, a GATA2 mollywhopper, if you will.
With that in mind, I don’t think it’s an exaggeration to say I was heavily invested in how this first appointment at MSK would go. I showed up with a four-page list of questions, most of which we didn’t even get to, but I was prepared. Prepared, at least, to maybe hear something I didn’t want to hear.

I’ll dive deeper into that appointment, the seemingly endless testing that took place after, and why I ultimately chose Dana-Farber instead of MSK in future posts, but here’s a brief summary of what I learned that day: We caught my condition early. To this day, I remain largely asymptomatic, and there are no signs in my DNA or elsewhere suggesting a high risk of relapse after the transplant. Essentially, if we tackle this aggressively and early, the odds are in my favor.
I can’t fully express what hearing that meant. It was a lifeline, pulling me from total uncertainty to something just a little less daunting. Sure, I still had plenty of questions, but anyone who’s ever been deep in the medical weeds before will understand how powerful that first piece of good news can be for your mental and physical well-being. I was a ball of stress during that time, still am honestly, but I’m managing it better now, as well as anyone can, I think, for being this close to transplant.
Closing Thoughts
So, that’s my diagnosis journey in a nutshell, my unofficial guide on how to get diagnosed with a rare genetic condition. While it felt confusing and overwhelming while I was in it, looking back, I can see there was a clear through-line. Each test and appointment built on the last, gradually leading me to the diagnosis and eventual treatment plan that I need.
What sets my experience apart, I think, is that I had time on my side. I wasn’t stuck in a hospital bed while doctors scrambled to figure things out. I had the chance to absorb it all, bit by bit, and the chance now to physically and mentally prepare myself for what lies ahead. For that, I’m truly grateful. Your body and your health are gifts, don’t ever forget that.

Next week, I’ll be sharing more about where my health stands heading into transplant. I’ve mentioned it before, but I’m fortunate to be in a good place right now. Over the past couple of years, I’ve worked to build a strong foundation, both in my health and in my habits, and I plan to lean on that throughout recovery. I’ll be diving into my current exercise and nutrition routines, and how I hope to use them to help get back on my feet post-transplant. The goal in sharing these details is to highlight just how much your pre-transplant health can influence your experience during treatment and beyond.
As always, I would love to hear from you. If you have questions or just want to say hi, don’t hesitate.
Talk soon,
– Ethan
Resources
External links directly referenced in this article:
- https://www.nytimes.com/2025/05/07/well/aging-longevity-peter-attia.html
- https://peterattiamd.com/
- https://peterattiamd.com/outlive/
- https://my.clevelandclinic.org/health/diseases/22831-vitamin-b12-deficiency
- https://kidshealth.org/en/parents/splenic-sequestration.html
- https://www.mayoclinic.org/tests-procedures/ana-test/about/pac-20385204
- https://hartfordhospital.org/services/cancer-care
- https://www.mayoclinic.org/diseases-conditions/aplastic-anemia/symptoms-causes/syc-20355015
- https://www.mayoclinic.org/diseases-conditions/myelodysplastic-syndrome/symptoms-causes/syc-20366977
- https://www.mskcc.org/about/innovative-collaborations/msk-alliance/hartford-healthcare-old/msk-alliance-faqs
Leave a comment