Today, I’ll be breaking down what the build up to transplant has looked like for me so far. While I went into detail in a previous post about the road to my diagnosis, I thought it made sense to dedicate a separate post to everything that came after. Specifically, the appointments and testing I’ve gone through since my diagnosis in January to prepare for my upcoming admission in early August.
This probably goes without saying, but pre-transplant testing serves several important purposes. Because treatment is such an intensive process, your care team needs to get an understanding of your baseline health and identify any potential problem areas ahead of time. That’s why it’s common to have a long list of appointments scheduled before treatment begins as it helps build a clear picture of where you are at.
To make things easier to follow, I’ll be breaking this post into sections, with each one covering a different category of testing that I’ve undergone in the lead-up to my admission date in a few weeks.

Also, because I don’t have data or records to share for some of the sections near the end, I decided to include a few photos from a recent drive I took down to Misquamicut, Rhode Island. Throughout all of this, making time for things I genuinely enjoy has done wonders for my mental health. Photography has always been something I love, and I plan on making it a big part of my documentation process once treatment begins.
Disclaimer: I’m strictly speaking from my own experience and the specific tests my care team decided were necessary for me. While some of this may overlap with what others go through, pre-transplant testing can vary quite a bit depending on the individual and their situation.
Bloodwork
I’ve talked quite a bit about bloodwork in previous posts, but I felt it was important to include it here too. If you are in a similar situation, you can expect to have blood drawn at nearly every appointment with your care team. While it isn’t a perfect measurement tool, it’s one of the best and least invasive ways for your team to monitor how your body is responding to what you may have going on.
As my care team in Hartford explained it to me, blood production in the body involves many steps, and bloodwork captures a snapshot of the “final” product. While that can be helpful, it doesn’t always tell the full story of what’s happening internally. There are several stages involved in the formation of healthy blood cells, and if there’s an issue at the root, it might not show up in your results right away. It often takes time for the problem to cause enough change for it to become detectable through standard labs.

In my case, the genetic mutation I have is known to primarily affect the bone marrow, so through regular bloodwork, my care team has been able to monitor how the mutation has been impacting my blood production. Fortunately, there haven’t been any drastic changes so far. If they didn’t already know there was a deeper issue at play, my blood counts alone might not have raised any major concerns.
But because there is an issue, and we’re aware of it, bloodwork has been the primary tool my team has used to monitor things as I’ve moved through my appointments over the past couple of months.
If I had to give one piece of advice for getting through blood draw after blood draw, it would be this: don’t look. Watching them take the blood won’t make it hurt any less, but avoiding the visual can actually go a long way in helping you manage the discomfort.
Heart & Lung Function
Turns out, being a runner doesn’t get you out of doing a few tests on your heart and lungs. Fair enough, I guess. To start, let’s talk about the heart.
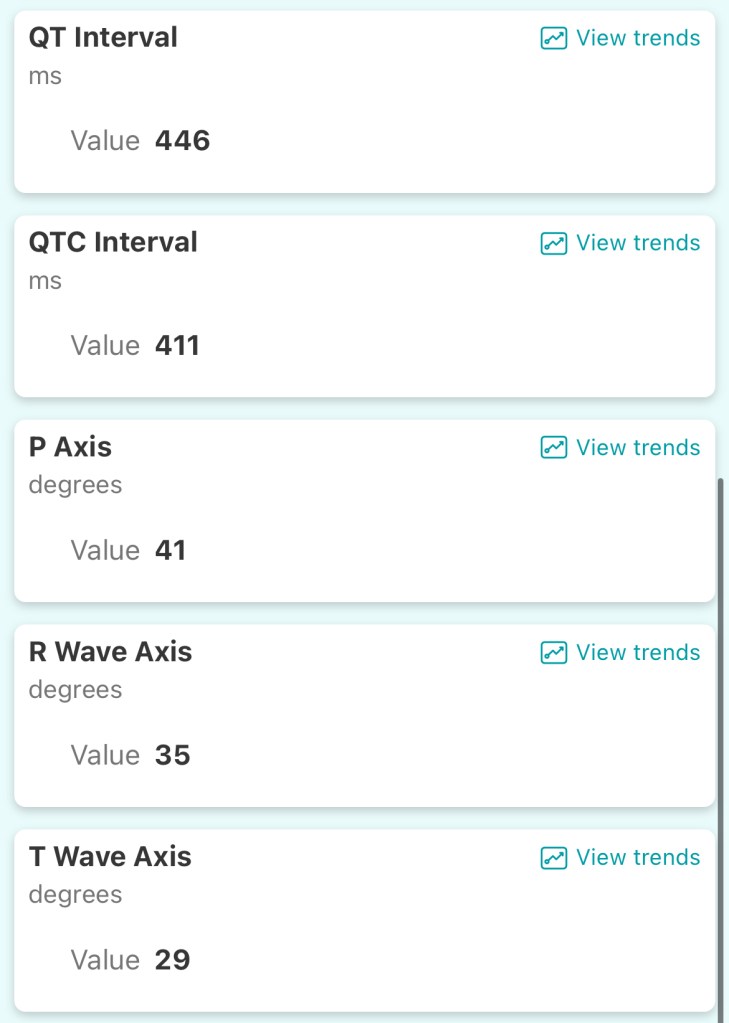
So far, I’ve only had two tests done to check how my heart is functioning: an EKG and an echocardiogram, both of which were done earlier this month. I chalk the lack of deeper testing of my heart up to being twenty-four and relatively healthy, aside from the genetic mutation that’s currently doing its best to ruin my life.
The EKG takes about 5 to 10 minutes and is pretty straightforward. Small electrical nodes are placed on your body to record the electrical signals your heart produces. It’s mainly used to detect heartbeat irregularities and similar issues.

An echocardiogram, on the other hand, is more like a traditional ultrasound. They apply that weird gel to your chest and use a handheld device to send sound waves that create images of your heart. It helps assess things like blood flow and valve function. The test usually takes 10 to 20 minutes, and while it’s relatively painless, it can get a little uncomfortable when the technician presses down on certain areas to get a clearer view.
Odds are you’ll be lying in an over-air-conditioned room, making small talk with the tech as they rub cold gel on your chest and throw around terms like “valve structure” and “diastolic function.” So really, complete comfort isn’t something you should count on.

Moving on to the lungs. When it comes to testing how well they function, I’m sad to report that the best option available is something called a pulmonary function test (PFT), otherwise known as the bane of my existence. A PFT involves a series of mildly complicated breathing exercises designed to measure how well your lungs move air in and out.
The data it captures is genuinely useful, but the quality of your results will depend on a few things: the health of your lungs (obviously), how clearly the instructions are explained, and your ability to follow said instructions.
I emphasize those last two points because the very first PFT I did back in January was pretty rough. Between the not-so-great instructions I received and my complete inability to grasp what was going on, the results ended up looking pretty concerning (see below).

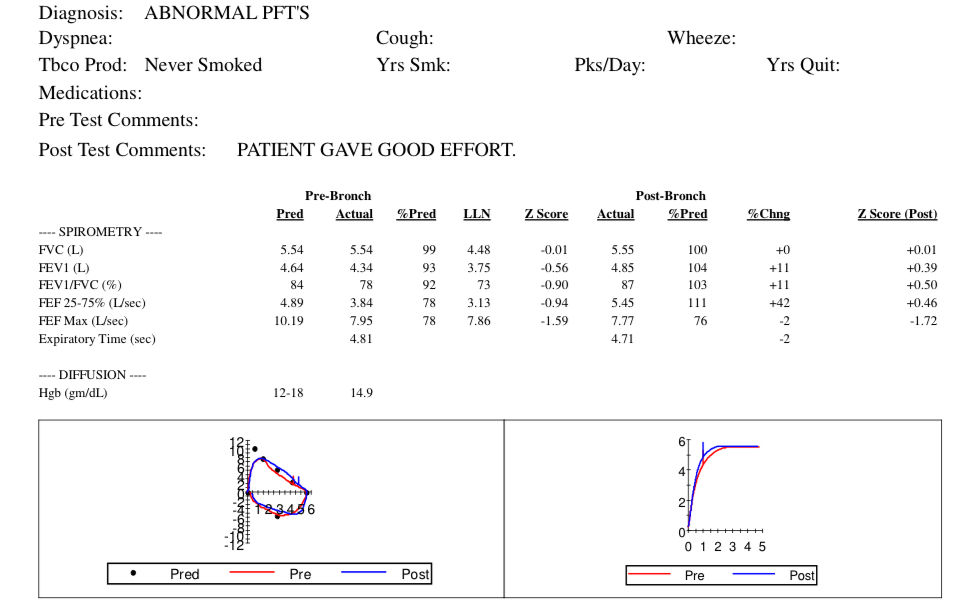
So concerning in fact that my pulmonologist suspected that if I retook the test and the results were similar, I might have undiagnosed asthma or an even more serious lung issue. Not exactly the kind of news you want to hear just four weeks after being diagnosed with a separate rare medical condition.
Luckily, shortly after that visit, I did retake the test with better instructions and a clearer understanding of what to do. That time, I passed with flying colors.
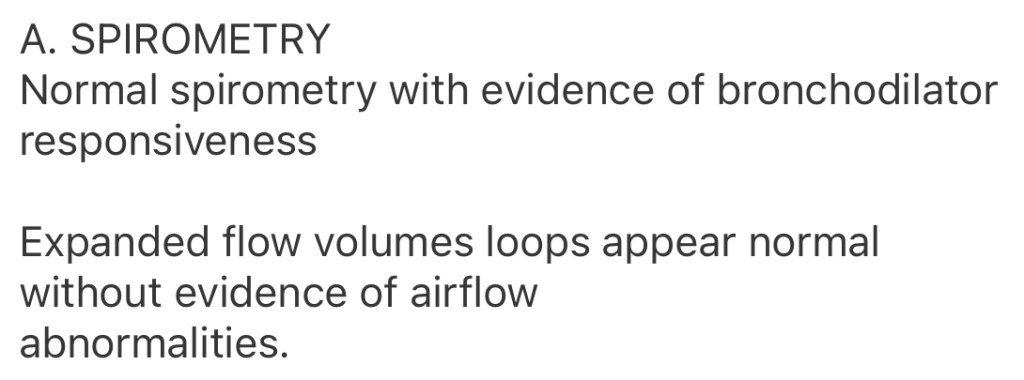
Earlier this month, during one of my longer visits to Dana-Farber, I completed one last PFT. It took about an hour, which I mostly blame on nerves. Out of all the tests I’ve done, the PFTs have been the toughest I think. Unlike most of the other pre-transplant tests, where I got to practice my dead log impression while someone poked me with a weird medical instrument, the PFTs demanded pretty active participation. I did well enough on two out of the three, but it definitely came at the cost of my sanity.
Imaging & Scans
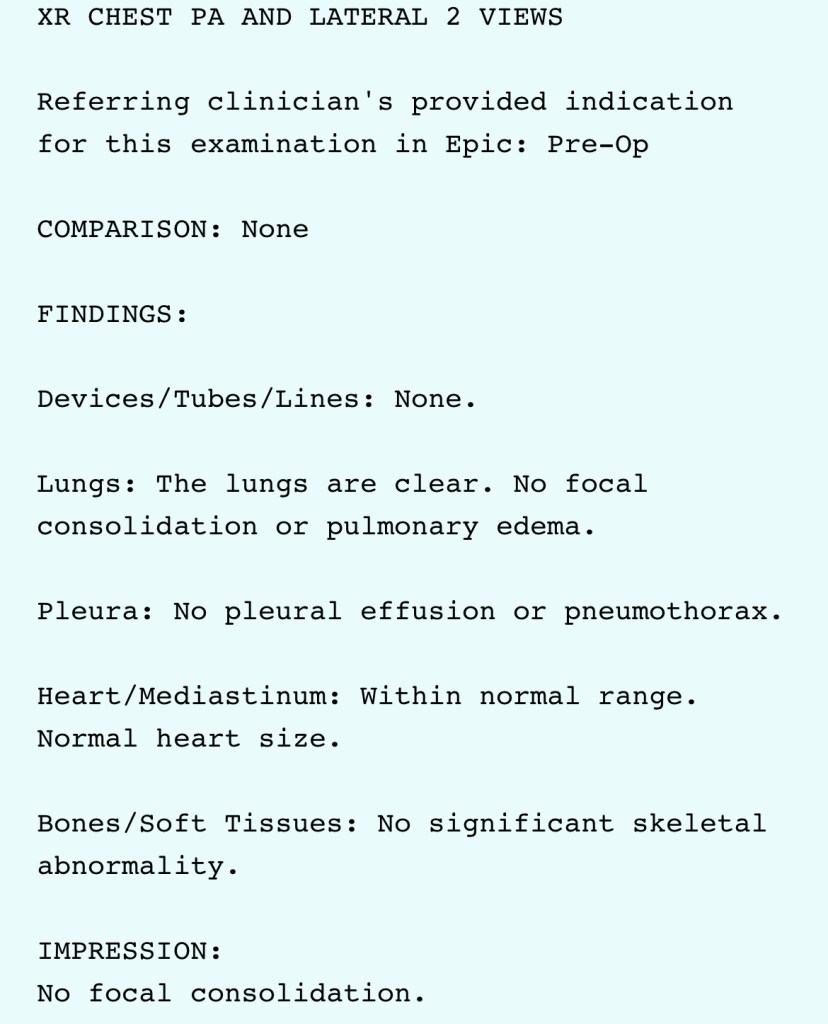
Imaging, overall, has been pretty minimal, which I’m definitely grateful for. So far, I’ve had two chest X-rays and a CT scan, all focused on my lungs.
The initial X-ray and CT scan were done around the same time earlier this year. While some pulmonologists might say the CT scan was a bit excessive, mine wanted to be sure we had a solid understanding of what shape my lungs were in before starting any kind of treatment or monitoring.

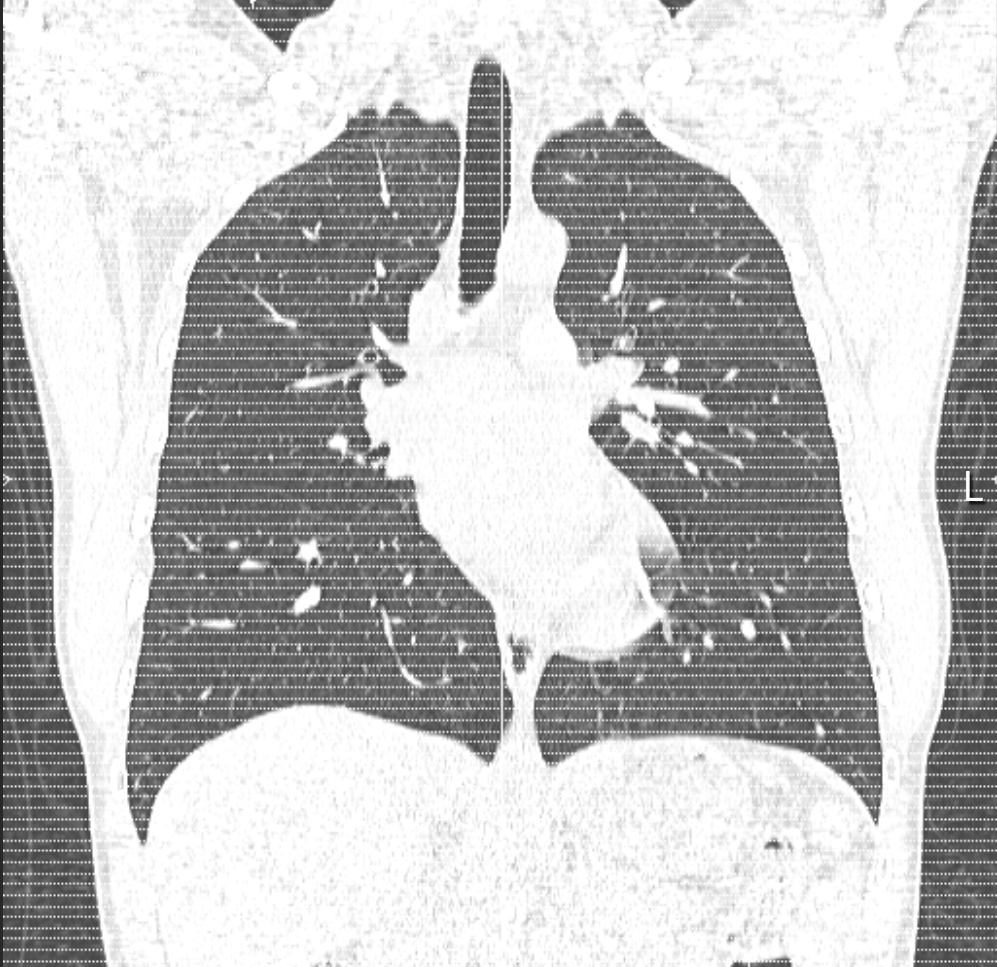
I agreed, because unfortunately, one of the other main areas the genetic mutation I have can affect is the lungs, so I wanted to make sure everything looked okay on that front. We also figured that it would be beneficial to have a baseline for comparison in case any issues come up down the line.
Both results (which I’ll share below) came back clear. I wasn’t expecting anything different, since I was still running without any issues, but it was still nice to get some good news at a time where it felt like good news was in short supply.
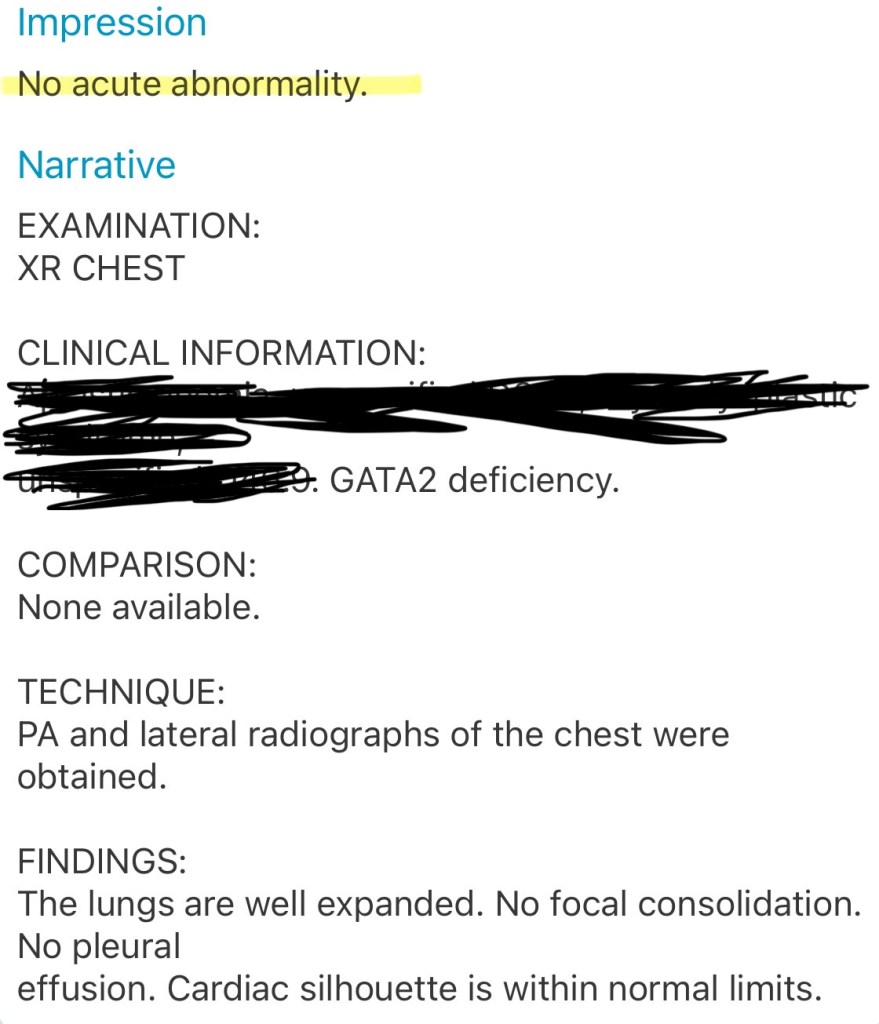
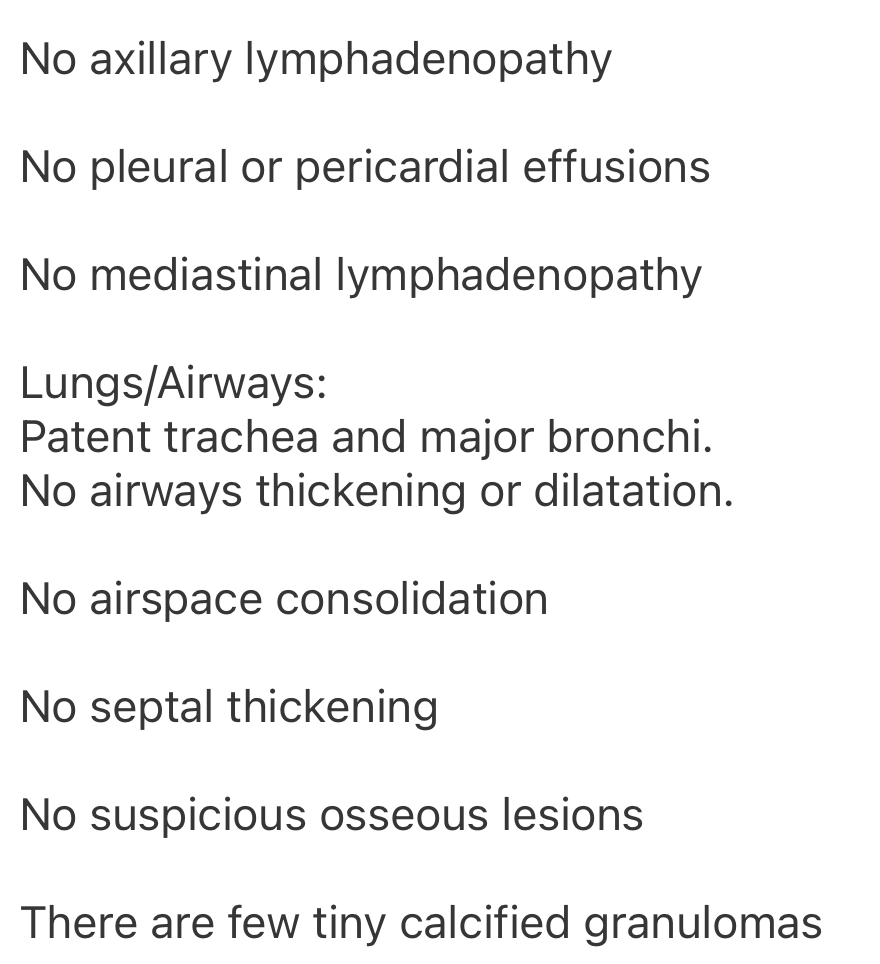
With my admission date approaching, we did one final chest X-ray a few weeks ago just to make sure everything still looked good, and it does. As you can imagine, being able to largely maintain my health throughout this whole process has meant a lot to me, and it’s always reassuring when the data backs that up.
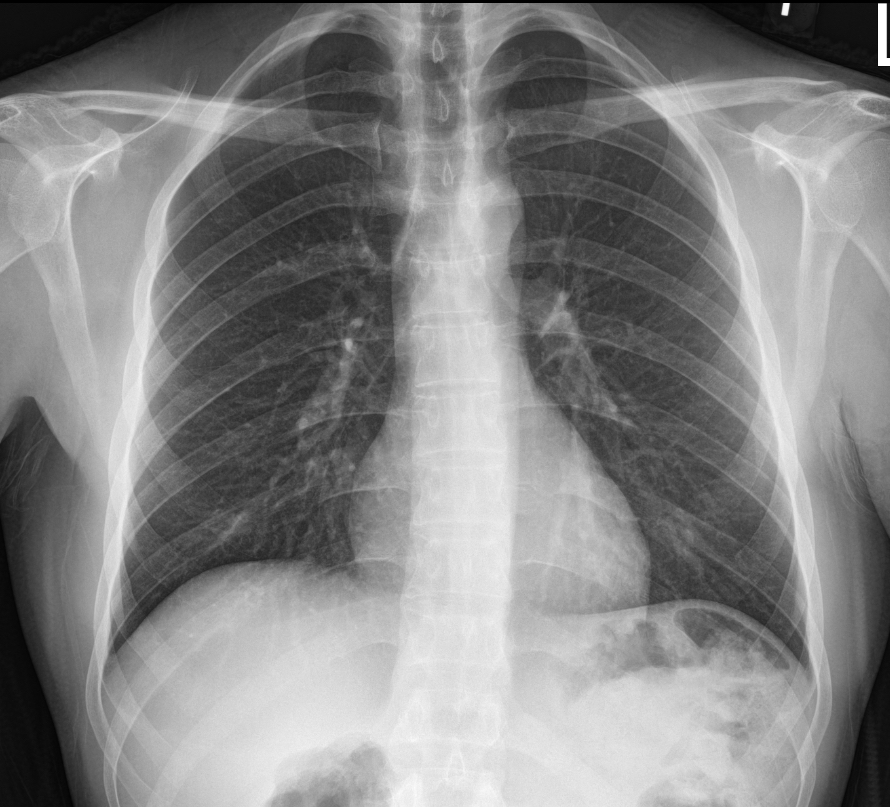
As for the actual experience, the X-rays felt quick and straightforward, but the CT scan was definitely more daunting. Even if you’re not claustrophobic, some discomfort is to be expected. The doughnut type machine they use is loud and definitely a little nerve-wracking, but I kept reminding myself they wouldn’t be putting me through it unless the information they were gathering was important.
Biopsies
Arguably the most invasive tests on the road to transplant are biopsies. Over the past 7 to 8 months, I’ve undergone two bone marrow biopsies and one skin punch biopsy.
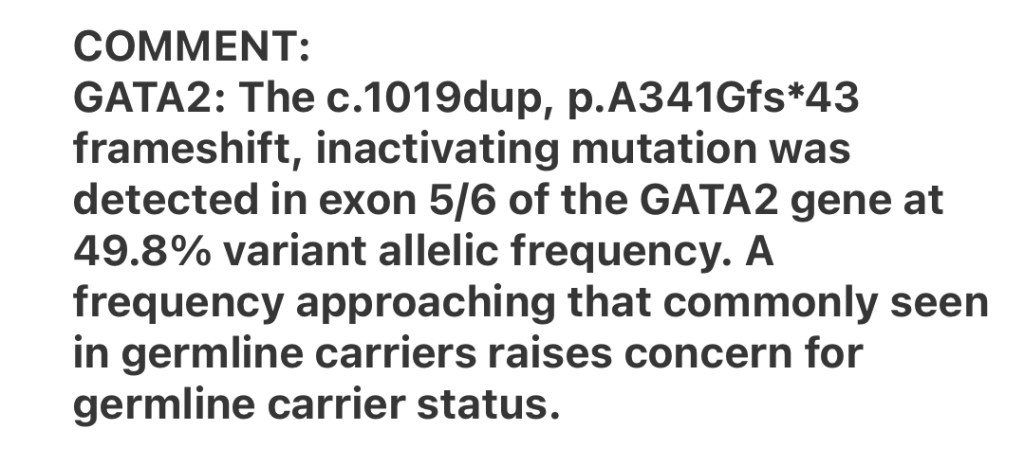
Starting with the skin punch biopsy, which I had done in February. This test was used to confirm my genetic mutation and figure out where it originated. Basically, they take a tiny piece of your skin using a cookie-cutter style tool (sorry for that visual) and analyze its genetic makeup.
I got to choose where they took the sample from, and I went with my upper thigh. The procedure was quick, but I won’t lie, there were definitely a moment or two when it stung. They stitched me up afterward and sent me on my way, and since I’m still here today, I guess it went well enough.
I’ve shared the results in a previous post, but I’ll include them again below. What I didn’t dive into last time was the origin of my mutation. According to my care team, it likely occurred when I was conceived, which technically makes it a germline mutation (In english: Hereditary). But, and this is a big but, luckily, no one else in my family has this mutation. Both my parents and my older brother all have normal copies of the GATA2 gene.

The GATA2 mutation I have is one of those “random” changes that can occur at conception regardless of the genetic makeup of your parents. Many of these changes are harmless and completely normal, but I happened to get one that was neither of those things.
And just to clear up any questions, the other two genetic variations listed in my results are known as variants of uncertain significance (VUS). Probably self explanatory, but there just isn’t enough information known about the specific variants to say whether or not they are anything to worry about. Each variant came from one of my parents, so there is no mystery with those ones.
Genetic testing can often be done through less invasive methods, which I highly recommend looking into if you’re curious about your own genetic situation. In my case, I needed this version of genetic testing because of my specific circumstance, but most genetic tests are done using blood draws, cheek swabs, or other similar more simple procedures.
Moving on, the first bone marrow biopsy, which I completed in December 2024, was what led to my diagnosis in January. It was done after most, if not all, other avenues had been explored to determine why my blood counts were lower than normal. While the biopsy experience can be daunting, I’ve had two very positive experiences so far, and I credit that to the skill and care of my medical team.

The medical professionals who perform these biopsies are exactly that, professionals. They’ve likely done hundreds or thousands of them, so you can take comfort in knowing you’re in very capable hands.
For both bone marrow biopsies, I was prescribed a small dose of Ativan, an anti-anxiety medication, to take before the procedure. If you’re feeling nervous or anxious, I recommend talking to your medical team about whether they can prescribe something similar. In many cases, they may offer it proactively, as they did for me, but it’s always good to ask just in case.

When the procedure begins, you’ll either lie on your stomach or your side. I was on my stomach both times. The first shot is usually the most painful, but things get more manageable after that. They’ll give you a few injections of numbing medication, each going a bit deeper, until they reach your hip bone.
When they go to extract the marrow, you may feel a bit of a pulling sensation that is not exactly pleasant, but it won’t last long. Before you know it, they’ll be cleaning up, and the procedure will be done.
The best part of all this is that you really can’t watch them do it. The same rule that applies for blood draws applies here as well. It doesn’t make it hurt less, but creating some distance between what is happening and what you can actually observe really does help.
I completed my second bone marrow biopsy in May, about five months after the first one in December. The results from that second biopsy are what ultimately led my care team to move forward with the transplant. There was just enough progression in my condition to make clear where things were heading without intervention.

Biopsies can be overwhelming and a little scary, there’s really no way around that. But like I reminded myself during the CT scan, data is a good thing. It’s what your care team relies on to give you the best possible treatment. Keeping that in mind can make the inevitable discomfort a bit easier to manage.
Dental
Teeth might not be top of mind on the road to transplant, but when they say everything matters, they really mean it. Before you can begin the treatment, you’ll need to pass a dental clearance exam.
The reasoning is pretty straightforward: you’re about to undergo intensive treatment with a mix of powerful medications, all of which come with potential side effects, not to mention the added risks that come with the transplant itself.

Infection is one of the main risks doctors will be on the lookout for throughout the transplant process, and since the mouth is a natural breeding ground for bacteria, it makes sense that they’d want you to show up with good oral health.
Because of that, any pre-existing issues will need to be addressed before transplant. One way they check for problems is through dental X-rays, which your transplant team will request and your dental team will use in conjunction with your dental exam results to decide if any work needs to be done.
Dentist visits aren’t exactly fun, but like every other test I’ve mentioned, they serve an important purpose: making sure your body is as ready as possible for transplant.
TL;DR: Floss. Seriously.

Fertility
This part isn’t all that easy to write about. At twenty-four, I always figured I’d have kids someday. I never expected there to be anything that might get in the way of that. But it turns out that getting diagnosed with a harmful genetic mutation and needing a stem cell transplant qualifies as one of those things.
During my most recent appointment at Dana-Farber, my doctors confirmed that undergoing this treatment will most likely make me infertile, meaning I won’t be able to have kids naturally after this.
I’ve been so focused on getting ready for treatment that I haven’t had the time or energy to really unpack how that fact has affected me. I can tell you it sucks, that much I know, but anything beyond that? I don’t have the words yet. And that’s okay I think.

What I can tell you, though, is that there are options. Ones I’ve taken advantage of to give myself the best chance of still having kids someday. For males, most transplant teams will recommend sperm banking before treatment begins. It’s the process of freezing a sperm sample for potential use in IVF down the line, should you and your partner decide to try for a child.
Obviously, I can only speak from the male perspective here. That said, I came across a page from the Mayo Clinic that has helped me better understand what fertility preservation might look like for both men and women. I’ll link it below in case you would like to have a look.

Because my genetic mutation is hereditary, and not something I acquired throughout my life, it exists in every cell of my body. While the transplant will effectively “cure” me by replacing the bone marrow where the mutation can cause damage, the mutation will still be a part of my genetic makeup. This means that in the unlikely scenario in which I remain fertile after treatment, should I try and have a child naturally, there is a 50/50 chance that the child would inherit my copy of the GATA2 gene.
Obviously, this is not something I want to pass on. Fortunately, through the IVF process, doctors can more or less ensure that any fertilized eggs carrying my copy of the GATA2 gene would not be used. I won’t pretend to fully understand the science behind it, so I’ll be linking an article below from the Cyprus American IVF Center that explains how this is possible in a bit more detail.
Mental Health
Last, but definitely not least, is the mental health aspect of all this. It could honestly be its own post, and I expect I’ll have a lot more to say on the topic as I move through treatment.
For now, there is not a lot that I feel that I can discuss confidently. What I can say is that there are plenty of resources available if you need support. Between my health insurance, my job’s Employee Assistance Program, and Dana-Farber, I’ve been offered several counseling options to turn to if I ever feel the need to talk.

At this point, I don’t feel the need to use those resources, but knowing there’s a whole network of people ready to support me if I do is very comforting.
There are also plenty of online resources you can take advantage of. One I’d like to highlight is the National Marrow Donor Program (NMDP), a global nonprofit that does a lot of great work in the blood disorder and blood cancer space. One of their key focus areas is supporting patients and their families throughout the transplant process. From start to finish and beyond.

While I may not have felt the need, Dana-Farber arranged for me to meet with one of their dedicated social workers for a visit or two. I believe it was mostly for insurance purposes, but both visits went very well.
It was nice to have someone to vent to who wasn’t a doctor in the traditional sense. Someone who was focused solely on my mental health rather than my physical health. A welcome break after about six months of talking to doctor after doctor about what was happening physically.
Closing Thoughts
So, that was a lot, I know. In this pre-transplant phase, it’s all about gathering as much useful data as possible. Not everything is glamorous, but it’s a crucial part of the process.
Hopefully, this post has given you a clearer idea of what to maybe expect in the lead-up to a stem cell transplant. As I mentioned earlier, everyone’s journey is different, and the transplant experience itself will vary from person to person. That said, the pre-transplant testing doctors perform is likely more consistent and streamlined across patients than the rest of the process.

My next post will focus more on the logistics behind my upcoming transplant. While my main job is simply to show up, there’s a lot of behind-the-scenes work involved in getting ready to do that. Things like paid leave, post-transplant housing, insurance, and more have all been carefully coordinated over the last couple of weeks/months to prepare me for my admission.
Through sharing those details, I hope to offer you a better sense of what you might need to consider before starting your own treatment journey, and the kind of preparation it takes to make sure everything is in place before things get underway.
As always, your questions and thoughts are more than welcome. I’d love to hear from you!
Talk Soon,
-Ethan
Resources
External links directly referenced in this article:
- https://my.clevelandclinic.org/health/diagnostics/24508-blood-tests
- https://www.researchgate.net/figure/Chart-of-haematopoiesis-15-Platelets-erythrocytes-polymorphonuclear-neutrophils_fig1_309730379
- https://www.mayoclinic.org/tests-procedures/ekg/about/pac-20384983
- https://www.mayoclinic.org/tests-procedures/echocardiogram/about/pac-20393856
- https://my.clevelandclinic.org/health/diagnostics/17966-pulmonary-function-testing
- https://www.mayoclinic.org/tests-procedures/bone-marrow-biopsy/about/pac-20393117
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/punch-biopsy
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/germline-mutation
- https://www.cdc.gov/genomics-and-health/counseling-testing/genetic-testing.html
- https://www.drugs.com/ativan.html
- https://www.ncbi.nlm.nih.gov/books/NBK65999/figure/CDR0000368374__342/
Fertility specific:
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/sperm-banking
- https://www.mayoclinic.org/tests-procedures/in-vitro-fertilization/about/pac-20384716
- https://www.mayoclinic.org/healthy-lifestyle/getting-pregnant/in-depth/fertility-preservation/art-20047512
- https://www.cyprusamericanivf.com/does-ivf-prevent-genetic-diseases/
Mental health specific:
Leave a comment